PATIENT EDUCATION
Frequently Asked Questions
Frequently Asked Questions
The Aorta
Aorta
What is an aorta?
The aorta is an artery and the largest blood vessel in the body. It carries oxygen-rich blood away from the heart to the body. Doctors refer to the upper part of the aorta as the thoracic aorta and the lower part as the abdominal (related to the belly) aorta.
Where is the aorta?
The aorta runs right down the middle of your body. But it doesn’t take a completely straight path.
It starts at the aortic valve, a special flap that connects the heart to the aorta. The aortic valve’s job is to keep blood from flowing backwards after it’s left the heart.
From there, the aorta stretches upwards, towards the neck. This section is called the ascending aorta.
Instead of continuing upwards, the aorta then forms a curve called the aortic arch.
By the end of that curve, the aorta is directed downwards. This portion is called the descending aorta.
The descending aorta travels down the chest and becomes the abdominal aorta when it crosses the diaphragm. The abdominal aorta comes to an end just above the groin, where it splits into two arteries, one for each leg. These are called the iliac arteries.
Why is the aorta important?
The aorta is important because it gives the body access to the oxygen-rich blood it needs to survive.
The heart itself gets oxygen from arteries that come off the ascending aorta.
The head (including the brain), neck and arms get oxygen from arteries that come off the aortic arch.
The stomach, intestines, kidneys and other vital organs get oxygen from arteries that come off the abdominal aorta.
How can you keep your aorta healthy?
Your aorta can be damaged by high cholesterol and high blood pressure, so anything you do to keep those risk factors under control will also help you maintain a healthy aorta.
That includes eating a balanced diet, getting regular exercise and avoiding cigarettes.
Types of Disease
Aortic Dissection
What is aortic dissection?
An aortic dissection is a small tear in the inner layer of the aortic wall that allows blood to flow between the layers.
Aortic dissections are classified into two types: type B dissection involves a tear in the descending part of the aorta and may extend into the abdomen, whereas type A dissection develops in the ascending part of the aorta just as it branches off the heart.
What are the symptoms of aortic dissection?
An aortic dissection has a sudden onset of symptoms similar to a heart attack; for example, symptoms may include:
- Sudden severe chest or upper back pain, often described as a tearing, ripping or shearing sensation that radiates to the neck or down the back
- Sudden severe abdominal pain
- Loss of consciousness
- Shortness of breath
- Sudden difficulty speaking, loss of vision, weakness or paralysis of one side of your body, like those of a stroke
- Weak pulse in one arm or thigh compared with the other
- Leg pain
- Difficulty walking
- Leg paralysis
If you experience any of the symptoms listed above, you should contact your doctor immediately.
How is aortic dissection treated?
Your doctor will determine your best method of treatment based on a number of factors such as your age, current state of health, the size of your dissection and how fast it is progressing.
Small dissections that are found early and not causing symptoms may not need immediate treatment or might be treated with medication.
Large or fast-growing dissections will need to be repaired to prevent a rupture. The standard method for repair is a traditional open surgical technique*. The extent of aorta that needs to be treated varies patient to patient.
*TEVAR is recommended as first line treatment for some dissections in suitable patients
Abdominal Aortic Aneurysm (AAA)
What is an abdominal aortic aneurysm?
The aorta is your body’s largest artery and carries oxygen-filled blood from your heart to all parts of your body. In your abdomen, the aorta splits into the iliac arteries, which carry blood to your legs and lower areas of your body and normally ranges in diameter from 3/4” to 1” (2–2.5 cm).
When an abnormal bulge or swelling occurs in your abdominal aorta, it is called an Abdominal Aortic Aneurysm or AAA. An aneurysm can increase in size. The larger the size of an aneurysm, the greater risk it could burst or rupture.
What are the symptoms of an abdominal aortic aneurysm?
Abdominal Aortic Aneurysms may go unnoticed initially because patients may not feel any symptoms, AAA are usually detected when doctors are ordering tests for other reasons.
When symptoms are experienced, the most common are:
- Pain in the chest, abdomen, flank or lower back, possibly spreading to the groin, buttocks, or legs.
- A pulsating sensation in the abdomen.
- Coldness, bruising or pain in your lower leg or foot can occur if the AAA produces a blood clot that breaks off and blocks blood flow.
- Fever or weight loss, if it is an inflamed/infected Abdominal Aortic Aneurysm.
If you experience any of the symptoms listed above, you should contact your doctor immediately.
How is a abdominal aortic aneurysm treated?
Treatment for an Abdominal Aortic Aneurysm depends on its size, location and your overall health. Together with your doctor, you will decide on the best option for treating your abdominal aneurysm.
If your doctor feels the aneurysm is at risk to burst or rupture, the treatment is generally either Open Surgery or Endovascular Aneursym Repair (EVAR), which is a less invasive treatment.
Thoracic Aortic Aneurysm (TAA)
What is a thoracic aortic aneurysm?
A thoracic aortic aneurysm (TAA) is a weakened and bulging area in the wall of the thoracic aorta (section of the aorta in the chest). TAAs can grow in size over time further weakening the wall of the aorta and may potentially burst or rupture (causing bleeding inside of the body).
As the aorta supplies the body with most of the oxygenated blood from the heart, a ruptured TAA can cause life-threatening bleeding.
What are the symptoms of a thoracic aortic aneurysm?
As a thoracic aortic aneurysm grows, some people may notice:
- Tenderness or pain in the chest,
- Back pain,
- Hoarseness,
- Cough,
- Shortness of breath
If you experience any of the symptoms listed above, you should contact your doctor immediately.
How is a thoracic aortic aneurysm treated?
Your doctor will determine your best method of treatment based on a number of factors such as your age, current state of health, the size of your aneurysm and how fast it is progressing.
Small aneurysms that are found early and not causing symptoms may not need immediate treatment or might be treated with medication.
Large or fast-growing aneurysms will need to be repaired to prevent a rupture. The standard method for repair is a traditional open surgical technique. The extent of aorta that needs to be treated varies patient to patient.
Blunt Traumatic Aortic Injury (BTAI)
What is a blunt traumatic aortic injury?
A Blunt Traumatic Aortic Injury (BTAI) is a tear in wall of the aorta. The tear may be a complete tear (a tear that goes through the whole wall of the aorta). This causes internal bleeding and is fatal in most cases. The tear may not be a complete tear of the wall of the aorta. The aorta is weakened at the location of the smaller or partial tear and may potentially be ballooned (similar to what is described in the aneurysm section). If the tear is not treated, the aorta could rupture resulting in life-threatening bleeding in the body.
What are the symptoms of a blunt traumatic aortic injury?
Most often, Blunt Traumatic Aortic Injury occurs because of blunt force trauma and massive deceleration (extremely fast stopping) that causes significant injury to the chest. For example, this may happen due to an car or motorcycle crash or a fall from a very high height.
How is a blunt traumatic aortic injury treated?
Your doctor will determine your best method of treatment based on a number of factors such as your age, current state of health, the size of your BTAI and how fast it is progressing.
Treatments
Open Surgical Repair
What is open surgical repair?
An open surgical repair is the traditional procedure used to repair a lesion or dissection.
Open repair surgery replaces the weak section of the aorta (the lesion) with a graft. This operation is successful in most cases. The graft usually works well for the rest of your life.
Your doctor only recommends this operation if they think that the risk of the lesion bursting is higher than the risk of having treatment.
What happens during open surgical repair?
In open surgery, the surgeon reaches the lesion through a large incision. The weakened section of the vessel, where the lesion has formed, is usually surgically replaced with a synthetic material.
Open surgery is usually performed under general anesthesia and takes several hours to complete. Repairing the lesion surgically requires an experienced vascular surgical team.
You will have a cut either down or across your abdomen. Occasionally, it is necessary to make a smaller cut on one or both sides of your groin.
After your surgery, you normally stay in the Intensive Care Unit (ICU) a day or two and then another five to seven days in the hospital, depending on how your body heals. Your recovery time may be about three to six months before you feel able to resume your normal activities.
What are the benefits of open surgical repair?
Open surgical repair is a well-proven surgical procedure seen as a standard method of treatment. With lasting results, the likelihood of having additional interventions decreases over time.
While long term follow-up with your surgeon is recommended, the imaging needed is not as frequent as required after Endovascular Repair. There is less radiation and contrast dye exposure thus decreasing the risk from imaging requirements.
What are the possible risks with open surgery?
Chest infections can occur following this type of surgery, particularly in smokers, and may require treatment with antibiotics and physiotherapy.
Slight discomfort and twinges of pain in your wound are normal for several weeks following surgery. Wounds sometimes become infected and these can usually be successfully treated with antibiotics. Also, the groin wound can fill with a fluid called lymph that may leak between the stitches but this usually decreases with time.
Occasionally, the bowel is slow to start working again, but fluids will be provided in a drip until your bowels return to normal. Sexual activity may be affected due to nerves in your abdomen being cut during the operation.
As with any major operation there are potential risks of medical complications. Your doctor will only recommend treatment for your aneurysm if they believes the risk of the aneurysm bursting is higher than the potential risk of an operation. Discuss with your surgeon the risk of:
- Heart attack
- Stroke
- Kidney failure
- Incision related complications
- Loss of circulation in the legs or bowel
- Infection in the graft used to replace your aorta
- General anesthesia
- Major abdominal surgery/long abdominal cut
- The surgical complication rate being higher than minimally invasive EVAR
- A longer hospital stay and recovery time than EVAR
- Blood loss during the procedure
- Deep vein thrombosis (DVT)
- Death
What will my recovery be like after open surgery?
After your surgery, you normally stay in the Intensive Care Unit (ICU) a day or two and then another five to seven days in the hospital, depending on how your body heals. Your recovery time may be about three to six months before you feel able to resume your normal activities.
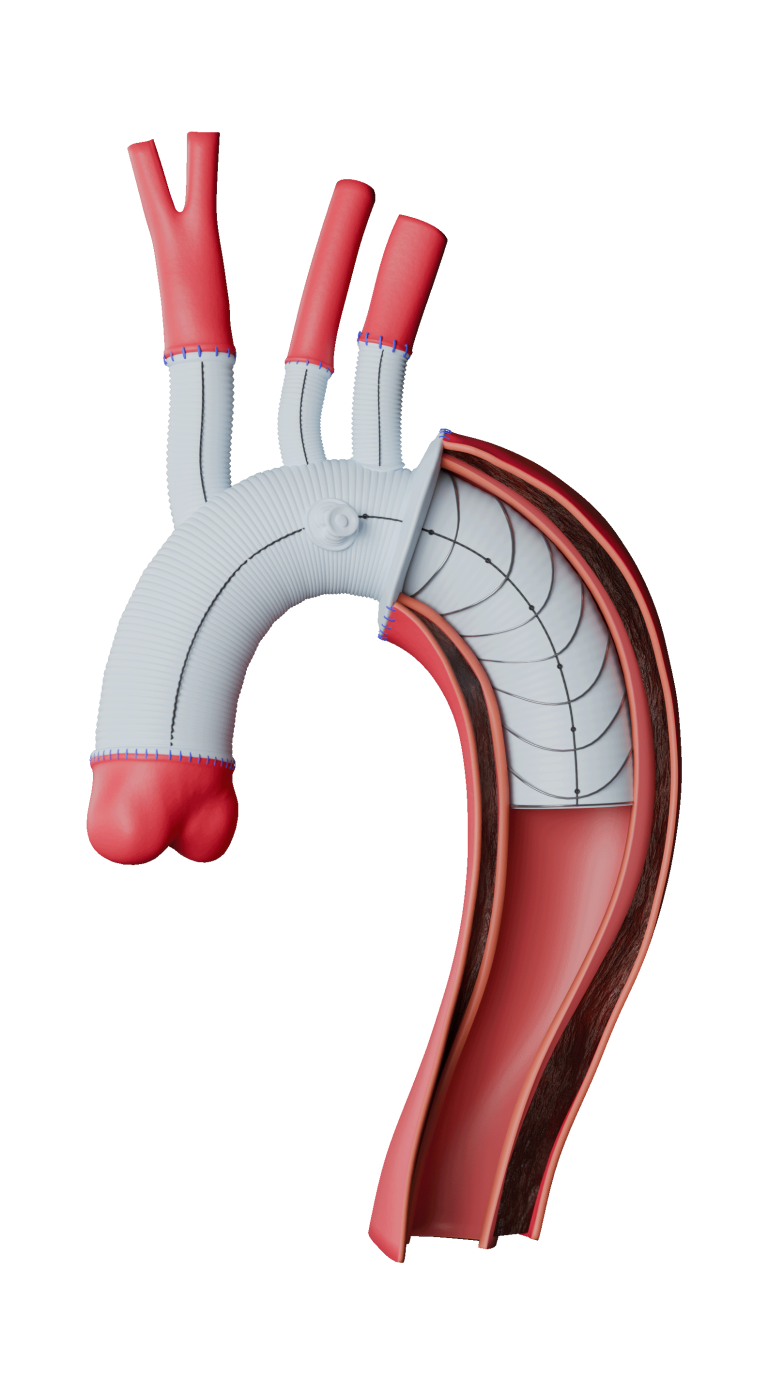
Endovascular Repair
What is endovascular repair?
Endovascular repair is a minimally-invasive surgery. It involves the use of a stent-graft that excludes (seals off) a lesion of a diseased aorta, thereby creating a new path for blood to flow.
A stent-graft is a fabric tube supported by a metal frame which is placed in the diseased aorta (section of your aorta where the lesion is located).
The stent-graft allows blood to flow normally through your aorta and is designed to protect the diseased aorta from blood pressure and flow.
The technique uses real time X-Rays allowing the doctor to visualise the location of the device and disease to ensure proper device placement. The doctor will also use a variety of other temporarily placed devices (such as guidewires) to perform the treatment.
What happens during an endovascular procedure?
Typically, endovascular repair takes 2 to 3 hours to complete. You will be asleep during the procedure and will not feel any pain. An overview of the procedure is briefly discussed below; please discuss any questions that you have on the procedure with your doctor.
- A small cut is made on one side of your groin.
- A delivery system is inserted into the opening and guided through your femoral artery to reach the part of your aorta that needs to be treated. Throughout the procedure, the doctor will view live x-ray pictures of your aorta to make sure the stent-graft is properly placed. This requires the use of dyes.
- Once the delivery system reaches the correct location, the stent-graft is deployed (expanded to its full size). When your stent-graft is released, it seals the aorta above and below the section where your disease/lesion is located from blood flow.
- The delivery system is removed from the body.
- Once the delivery system is removed, the doctor will recheck that your stent-graft is working properly.
- The opening in the groin is closed and the procedure is complete.
What are the benefits of endovascular repair?
As endovascular repair is less traumatic than open surgery, benefits may include:
- Minimally invasive procedure
- May be performed under local anesthesia
- Lower procedural complication rate as compared to open surgery
- May reduce the risk of a blood transfusion being required
- Less time may be spent in the intensive care unit after surgery
- Shorter average hospital stay
- Quicker recovery time than open surgical repair
What are the possible risks of endovascular repair?
As with any endovascular repair, repair with a stent-graft comes with potential risks. Please discuss all risks with your doctor. Major risks associated with endovascular stent-grafts include, but are not limited to:
- Endoleak – when blood continues to flow into the lesion
- Migration – movement of the stent-graft from its original position
- Device-related issues such as breaking of the sutures or metal portion of the stent- graft, fabric defects/tears or component separation
- Continued growth of the lesion
- Aortic rupture
- Additional endovascular or surgical procedures
- Heart attack
- Stroke
- Stent-graft thrombus
- Paraplegia
- Kidney failure
- Access site incision complications
- Conversion to open surgical repair
- Death
What will my recovery be like after endovascular repair?
Immediately after treatment
Immediately after recovery from the stent-graft procedure you may be required to lie flat for 4 to 6 hours. This allows for the healing to begin in your groin. Some patients experience mild discomfort such as swelling of the groin area or fever, but this usually resolves in a few days.
Other side effects may include:
- Numbness of the legs
- Nausea
- Vomiting
- Leg pain or throbbing
- Lack of appetite
- Endoleak (blood flow into the abdominal aortic aneurysm after placement of a stent-graft)
- Absence of bowel movement for 1 to 3 days
Follow-up
Your doctor will discuss your follow-up plan. Endovascular repair requires that you maintain regular lifelong follow-up with your doctor to ensure that the device is working properly. Some problems do not show symptoms and are not felt by the patient.
During your follow-up examinations, you may routinely receive:
- X-rays
- CT Scans
- Physical examinations
- Blood tests
- Ultrasound or MRI scans
Resources
Disclaimer
Our patient education hub gives only general information for patients. Your medical practitioner will be able to answer any specific questions you may have on your condition.
This information was produced as a service to medicine by Terumo Aortic.
Product availability subject to regulatory approval.
Instructions for Use
View the eIFU for more information on use, indications, contraindications, warnings/precautions and availability within your market.
Contact us
Click the button below to get in touch. For more updates, follow us on X and LinkedIn. You can also view our VuMedi channel.